| << Chapter < Page | Chapter >> Page > |
As noted earlier, normal oral microbiota can cause dental and periodontal infections. However, there are number of other infections that can manifest in the oral cavity when other microbes are present.
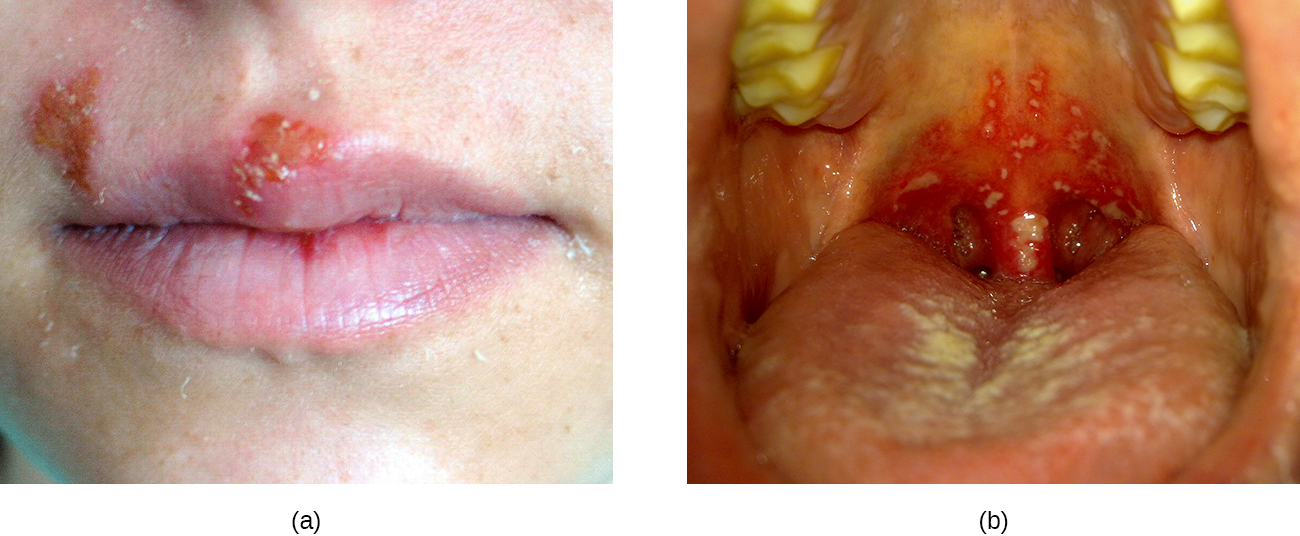
As described in Viral Infections of the Skin and Eyes , infections by herpes simplex virus type 1 (HSV-1) frequently manifest as oral herpes , also called acute herpes labialis and characterized by cold sores on the lips, mouth, or gums. HSV-1 can also cause acute herpetic gingivostomatitis , a condition that results in ulcers of the mucous membranes inside the mouth ( [link] ). Herpetic gingivostomatitis is normally self-limiting except in immunocompromised patients. Like oral herpes, the infection is generally diagnosed through clinical examination, but cultures or biopsies may be obtained if other signs or symptoms suggest the possibility of a different causative agent. If treatment is needed, mouthwashes or antiviral medications such as acyclovir , famciclovir , or valacyclovir may be used.
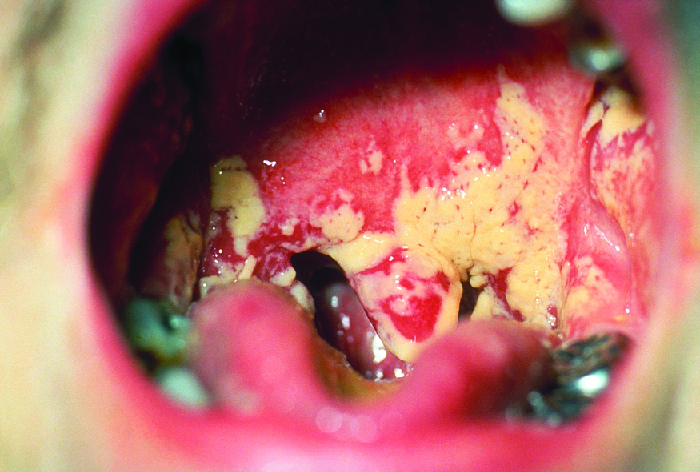
The yeast Candida is part of the normal human microbiota, but overgrowths, especially of Candida albicans , can lead to infections in several parts of the body. When Candida infection develops in the oral cavity, it is called oral thrush . Oral thrush is most common in infants because they do not yet have well developed immune systems and have not acquired the robust normal microbiota that keeps Candida in check in adults. Oral thrush is also common in immunodeficient patients and is a common infection in patients with AIDS.
Oral thrush is characterized by the appearance of white patches and pseudomembranes in the mouth ( [link] ) and can be associated with bleeding. The infection may be treated topically with nystatin or clotrimazole oral suspensions, although systemic treatment is sometimes needed. In serious cases, systemic azoles such as fluconazole or itraconazole (for strains resistant to fluconazole), may be used. Amphotericin B can also be used if the infection is severe or if the Candida species is azole-resistant.
The viral disease mumps is an infection of the parotid glands, the largest of the three pairs of salivary glands ( [link] ). The causative agent is mumps virus (MuV), a paramyxovirus with an envelope that has hemagglutinin and neuraminidase spikes. A fusion protein located on the surface of the envelope helps to fuse the viral envelope to the host cell plasma membrane.
Mumps virus is transmitted through respiratory droplets or through contact with contaminated saliva, making it quite contagious so that it can lead easily to epidemics. It causes fever, muscle pain, headache, pain with chewing, loss of appetite, fatigue, and weakness. There is swelling of the salivary glands and associated pain ( [link] ). The virus can enter the bloodstream ( viremia ), allowing it to spread to the organs and the central nervous system. The infection ranges from subclinical cases to cases with serious complications, such as encephalitis , meningitis , and deafness. Inflammation of the pancreas, testes, ovaries, and breasts may also occur and cause permanent damage to those organs; despite these complications, a mumps infection rarely cause sterility.
Mumps can be recognized based on clinical signs and symptoms, and a diagnosis can be confirmed with laboratory testing. The virus can be identified using culture or molecular techniques such as RT-PCR. Serologic tests are also available, especially enzyme immunoassays that detect antibodies. There is no specific treatment for mumps, so supportive therapies are used. The most effective way to avoid infection is through vaccination. Although mumps used to be a common childhood disease, it is now rare in the United States due to vaccination with the measles, mumps, and rubella (MMR) vaccine.

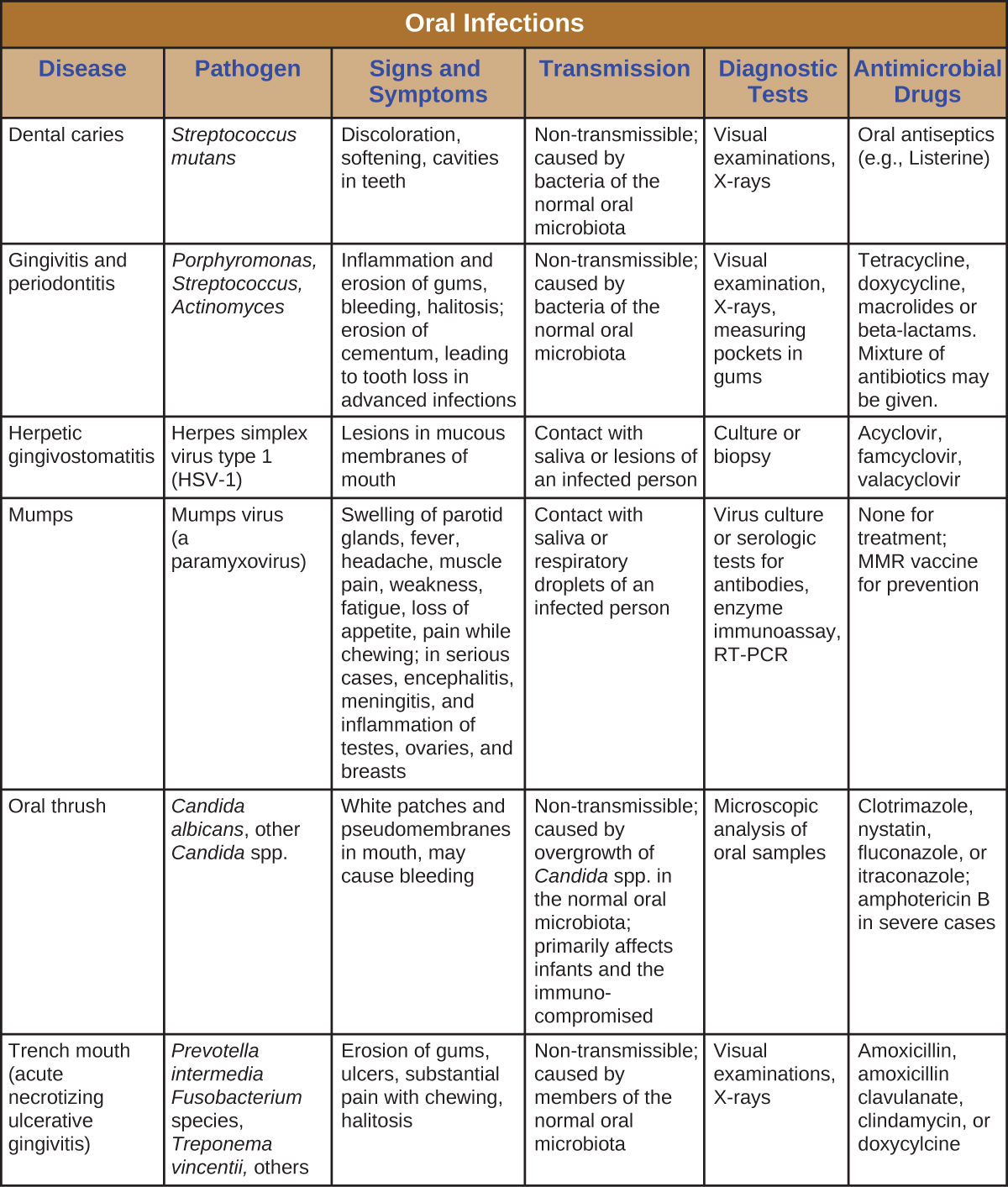
Infections of the mouth and oral cavity can be caused by a variety of pathogens, including bacteria, viruses, and fungi. Many of these infections only affect the mouth, but some can spread and become systemic infections. [link] summarizes the main characteristics of common oral infections.
When plaque becomes heavy and hardened, it is called dental calculus or _________.
tartar
Why do sugary foods promote dental caries?

Notification Switch
Would you like to follow the 'Microbiology' conversation and receive update notifications?