| << Chapter < Page | Chapter >> Page > |
Hepatocytes work non-stop, but bile production increases when fatty chyme enters the duodenum and stimulates the secretion of the gut hormone secretin. Between meals, bile is produced but conserved. Bile is diverted to the gallbladder, where it is concentrated and stored until the next meal.
The soft, oblong, glandular pancreas lies nestled into the “c-shaped” curvature of the duodenum with the body extending to the left. It is a curious mix of exocrine (secreting digestive enzymes) and endocrine (releasing hormones into the blood) functions ( [link] ). The exocrine part of the pancreas arises as little grape-like cell clusters, each called an acinus (plural = acini), located at the terminal ends of pancreatic ducts. These acinar cells secrete enzyme-rich pancreatic juice into tiny merging ducts that form two dominant ducts. The larger duct fuses with the common bile duct (carrying bile from the liver and gallbladder) just before entering the duodenum via a common opening. Scattered through the sea of exocrine acini are small islands of endocrine cells, the islets of Langerhans . These vital cells produce the hormones insulin, glucagon, and other crucial hormones.
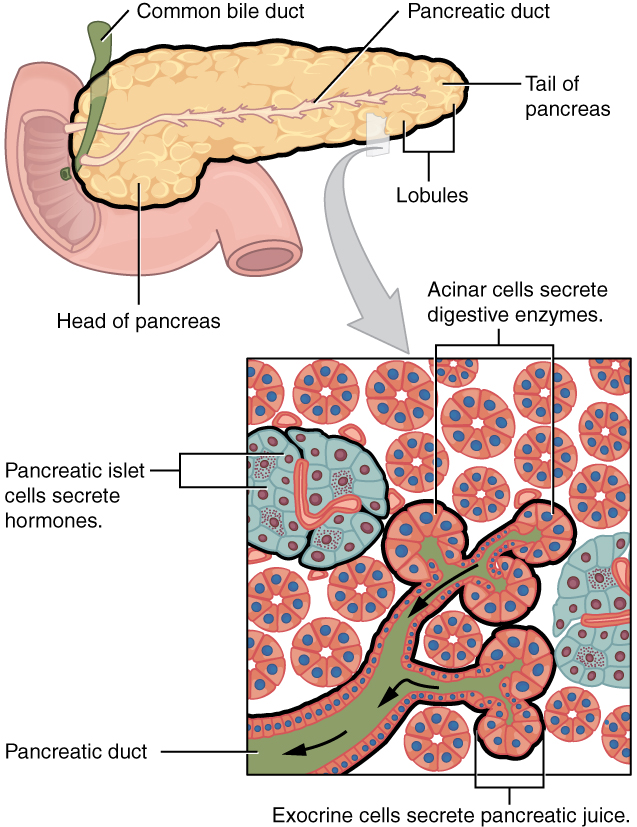
The pancreas produces over a liter of pancreatic juice each day. Unlike bile, it is clear and composed mostly of water along with some salts, sodium bicarbonate, and several digestive enzymes. Sodium bicarbonate is responsible for the slight alkalinity of pancreatic juice, which serves to buffer the acidic gastric juice in chyme, inactivate pepsin from the stomach, and create an optimal environment for the activity of pH-sensitive digestive enzymes in the small intestine. Pancreatic enzymes are active in the digestion of sugars, proteins, and fats.
The pancreas produces protein-digesting enzymes in their inactive forms. These enzymes are activated in the duodenum. If produced in an active form, they would digest the pancreas (which is exactly what occurs in the disease, pancreatitis).The enzymes that digest starch (amylase), fat (lipase), and nucleic acids (nuclease) are secreted in their active forms, since they do not attack the pancreas as do the protein-digesting enzymes.
Regulation of pancreatic secretion is the job of hormones. The entry of acidic chyme into the duodenum stimulates the release of the hormone secretin , which in turn causes the duct cells to release bicarbonate-rich pancreatic juice. The presence of proteins and fats in the duodenum stimulates the secretion of the hormone CCK , which then stimulates the acini to secrete enzyme-rich pancreatic juice and enhances the activity of secretin.
The gallbladder is 3–4 inches long and is nested in a shallow area on the posterior aspect of the right lobe of the liver. This muscular sac stores, concentrates, and, when stimulated, propels the bile into the duodenum via the common bile duct. The cystic duct is 1–2 cm (less than 1 in) long and merges with the hepatic duct coming from the liver. The gallbladder's mucosa absorbs water and ions from bile, concentrating it by up to 10-fold and storing the bile until it is needed.
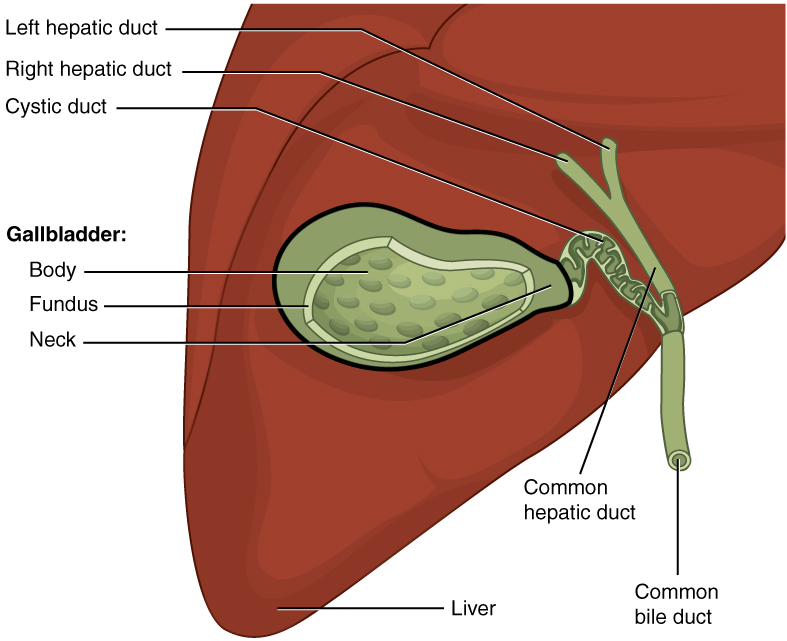
Chemical digestion in the small intestine cannot occur without the help of the liver and pancreas. The liver produces bile and delivers it to the common hepatic duct. Bile contains bile salts and phospholipids, which emulsify large lipid globules into tiny lipid droplets, a necessary step in lipid digestion and absorption. The gallbladder stores and concentrates bile, releasing it when it is needed by the small intestine.
The pancreas produces the enzyme- and bicarbonate-rich pancreatic juice and delivers it to the small intestine through ducts. Pancreatic juice buffers the acidic gastric juice in chyme, inactivates pepsin from the stomach, and enables the optimal functioning of digestive enzymes in the small intestine.

Notification Switch
Would you like to follow the 'Digestive system' conversation and receive update notifications?