| << Chapter < Page | Chapter >> Page > |
If no fertilized egg is implanted into the uterus, the corpus luteum degenerates and the levels of estrogen and progesterone decrease. The endometrium begins to degenerate as the progesterone levels drop, initiating the next menstrual cycle. The decrease in progesterone also allows the hypothalamus to send GnRH to the anterior pituitary, releasing FSH and LH and starting the cycles again.
Pregnancy begins with the fertilization and implantation of an egg and continues through to the birth of the individual. The length of time of gestation, or the gestation period, in humans is 266 days and is similar in other great apes. Gestation periods in other animals range from 12-13 days in the American opossum to the 660 day gestation period of the African elephant.
Within 24 hours of fertilization, the egg nucleus has finished meiosis and the egg and sperm nuclei fuse. With fusion, the cell is known as a zygote. The zygote initiates cleavage and the developing embryo travels through the oviduct to the uterus. The developing embryo must implant into the wall of the uterus within seven days, or it will deteriorate and die. The outer layers of the developing embryo or blastocyst grow into the endometrium by digesting the endometrial cells, and healing of the endometrium closes up the blastocyst into the tissue. Another layer of the blastocyst, the chorion, begins releasing a hormone called human beta chorionic gonadotropin (β-HCG) , which makes its way to the corpus luteum and keeps that structure active. This ensures adequate levels of progesterone that will maintain the endometrium of the uterus for the support of the developing embryo. Pregnancy tests determine the level of β-HCG in urine or serum. If the hormone is present, the test is positive.
The gestation period is divided into three equal periods or trimesters. During the first two-to-four weeks of the first trimester, nutrition and waste are handled by the endometrial lining through diffusion. As the trimester progresses, the outer layer of the embryo begins to merge with the endometrium, and the placenta forms. The placenta takes over the nutrient and waste requirements of the embryo and fetus, with the mother’s blood passing nutrients to the placenta and removing waste from it. Chemicals from the fetus, such as bilirubin, are processed by the mother’s liver for elimination. Some of the mother’s immunoglobulins will pass through the placenta, providing passive immunity against some potential infections.
Internal organs and body structures begin to develop during the first trimester. By five weeks, limb buds, eyes, the heart, and liver have been basically formed. By eight weeks, the term fetus applies, and the body is essentially formed ( [link] a ). The individual is about five centimeters (two inches) in length and many of the organs, such as the lungs and liver, are not yet functioning. Exposure to any toxins is especially dangerous during the first trimester, as all of the body’s organs and structures are going through initial development. Anything that interferes with chemical signaling during that development can have a severe effect on the fetus’ survival.
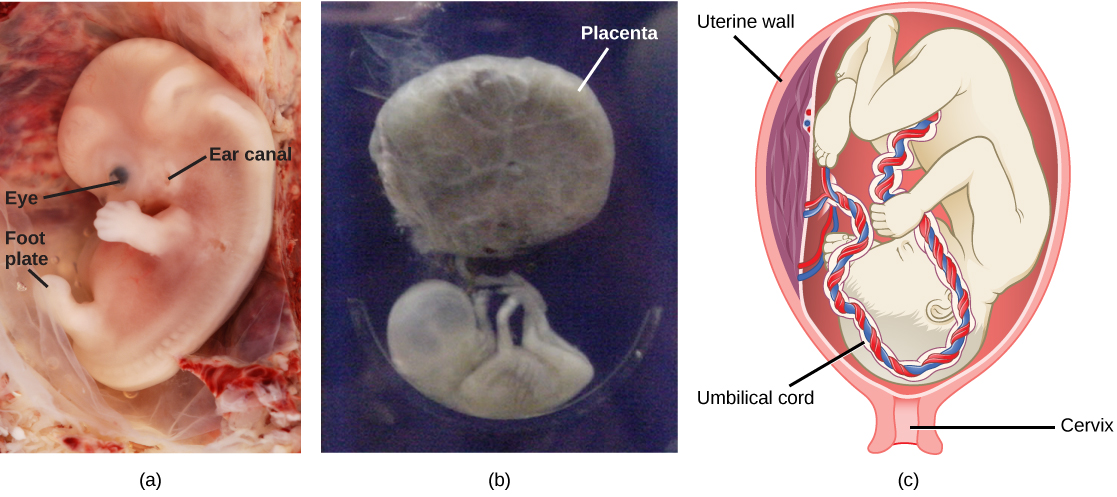
During the second trimester, the fetus grows to about 30 cm (about 12 inches) ( [link] b ). It becomes active and the mother usually feels the first movements. All organs and structures continue to develop. The placenta has taken over the functions of nutrition and waste elimination and the production of estrogen and progesterone from the corpus luteum, which has degenerated. The placenta will continue functioning up through the delivery of the baby. During the third trimester, the fetus grows to 3 to 4 kg (6.5–8.5 lbs.) and about 50 cm (19–20 inches) long ( [link] c ). This is the period of the most rapid growth during the pregnancy as all organ systems continue to grow and develop.
Labor is the name given to the muscular contractions that expel the fetus and placenta from the uterus. Toward the end of the third trimester, estrogen causes receptors on the uterine wall to develop and bind the hormone oxytocin. At this time, the fetus usually reorients, facing forward and down with the back or crown of the head pushing on the cervix (uterine opening). This causes the cervix to stretch and nerve impulses are sent to the hypothalamus, which signals the release of oxytocin from the posterior pituitary. Oxytocin causes smooth muscle in the uterine wall to contract. At the same time, the placenta releases prostaglandins into the uterus, increasing the contractions. A positive feedback relay occurs between the uterus, hypothalamus, and the posterior pituitary to assure an adequate supply of oxytocin. As more smooth muscle cells are recruited, the contractions increase in intensity and force. As noted previously, this is a good example of a positive feedback loop ‒ the stimulus causes the production of a hormone that increases the stimulus.
There are three stages to labor. During stage one, the cervix thins and dilates. This is necessary for the baby and placenta to be expelled during birth. The cervix will eventually dilate to about 10 cm. During stage two, the baby is expelled from the uterus. The uterus contracts and the mother pushes as she compresses her abdominal muscles to aid the delivery. The last stage is the passage of the placenta after the baby has been born and the organ has completely disengaged from the uterine wall. If labor should stop before stage two is reached, synthetic oxytocin, known as Pitocin, can be administered to restart and maintain labor.

Notification Switch
Would you like to follow the 'Principles of biology' conversation and receive update notifications?