| << Chapter < Page | Chapter >> Page > |
Immunity to pathogens, and the ability to control pathogen growth so that damage to the tissues of the body is limited, can be acquired by (1) the active development of an immune response in the infected individual or (2) the passive transfer of immune components from an immune individual to a nonimmune one. Both active and passive immunity have examples in the natural world and as part of medicine.
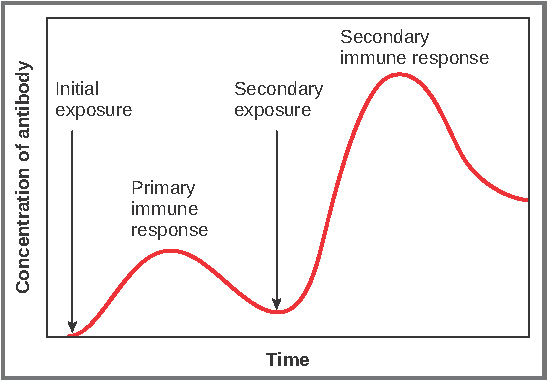
Active immunity is the resistance to pathogens acquired during an adaptive immune response within an individual ( [link] ). Naturally acquired active immunity, the response to a pathogen, is the focus of this chapter. Artificially acquired active immunity involves the use of vaccines. A vaccine is a killed or weakened pathogen or its components that, when administered to a healthy individual, leads to the development of immunological memory (a weakened primary immune response) without causing much in the way of symptoms. Thus, with the use of vaccines, one can avoid the damage from disease that results from the first exposure to the pathogen, yet reap the benefits of protection from immunological memory. The advent of vaccines was one of the major medical advances of the twentieth century and led to the eradication of smallpox and the control of many infectious diseases, including polio, measles, and whooping cough.
| Active versus Passive Immunity | ||
|---|---|---|
| Natural | Artificial | |
| Active | Adaptive immune response | Vaccine response |
| Passive | Trans-placental antibodies/breastfeeding | Immune globulin injections |
Passive immunity arises from the transfer of antibodies to an individual without requiring them to mount their own active immune response. Naturally acquired passive immunity is seen during fetal development. IgG is transferred from the maternal circulation to the fetus via the placenta, protecting the fetus from infection and protecting the newborn for the first few months of its life. As already stated, a newborn benefits from the IgA antibodies it obtains from milk during breastfeeding. The fetus and newborn thus benefit from the immunological memory of the mother to the pathogens to which she has been exposed. In medicine, artificially acquired passive immunity usually involves injections of immunoglobulins, taken from animals previously exposed to a specific pathogen. This treatment is a fast-acting method of temporarily protecting an individual who was possibly exposed to a pathogen. The downside to both types of passive immunity is the lack of the development of immunological memory. Once the antibodies are transferred, they are effective for only a limited time before they degrade.
Immunity can be acquired in an active or passive way, and it can be natural or artificial. Watch this video to see an animated discussion of passive and active immunity. What is an example of natural immunity acquired passively?
As discussed previously, Th2 cells secrete cytokines that drive the production of antibodies in a B cell, responding to complex antigens such as those made by proteins. On the other hand, some antigens are T cell independent. A T cell-independent antigen usually is in the form of repeated carbohydrate moieties found on the cell walls of bacteria. Each antibody on the B cell surface has two binding sites, and the repeated nature of T cell-independent antigen leads to crosslinking of the surface antibodies on the B cell. The crosslinking is enough to activate it in the absence of T cell cytokines.
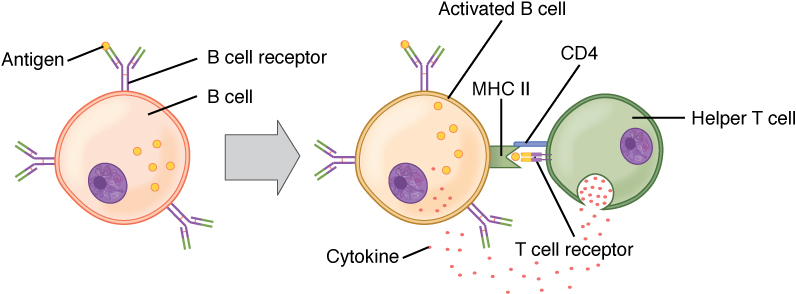
A T cell-dependent antigen , on the other hand, usually is not repeated to the same degree on the pathogen and thus does not crosslink surface antibody with the same efficiency. To elicit a response to such antigens, the B and T cells must come close together ( [link] ). The B cell must receive two signals to become activated. Its surface immunoglobulin must recognize native antigen. Some of this antigen is internalized, processed, and presented to the Th2 cells on a class II MHC molecule. The T cell then binds using its antigen receptor and is activated to secrete cytokines that diffuse to the B cell, finally activating it completely. Thus, the B cell receives signals from both its surface antibody and the T cell via its cytokines, and acts as a professional antigen-presenting cell in the process.
B cells, which develop within the bone marrow, are responsible for making five different classes of antibodies, each with its own functions. B cells have their own mechanisms for tolerance, but in peripheral tolerance, the B cells that leave the bone marrow remain inactive due to T cell tolerance. Some B cells do not need T cell cytokines to make antibody, and they bypass this need by the crosslinking of their surface immunoglobulin by repeated carbohydrate residues found in the cell walls of many bacterial species. Others require T cells to become activated.
Immunity can be acquired in an active or passive way, and it can be natural or artificial. Watch this video to see an animated discussion of passive and active immunity. What is an example of natural immunity acquired passively?
Breastfeeding is an example of natural immunity acquired passively.

Notification Switch
Would you like to follow the 'Anatomy & Physiology' conversation and receive update notifications?